Bunions rarely arrive overnight. They build slowly, with the big toe edging toward its neighbor and a bony prominence forming at the base joint. At first it is a mild hot spot in dress shoes or after a long day on your feet. Then it starts dictating your footwear, your mileage, even your willingness to walk a few blocks to dinner. I have seen people plan vacations around whether they can stand the sightseeing. If this sounds familiar, you are not alone. The question is not just how to quiet the pain, but when to involve a foot and ankle bunion surgeon and what that decision entails.
This guide walks through how bunions behave, what conservative care can accomplish, when surgery earns its keep, and how to choose the right foot and ankle specialist for your goals. The focus is pragmatic: what works in real clinics, for real people with jobs, hobbies, and timelines.
What a Bunion Actually Is, and Why That Matters
A bunion is not just a bump. It is a progressive deformity of the first metatarsophalangeal joint, the big toe’s base. The long metatarsal bone drifts inward, the toe drifts outward, and the joint capsule on the inner side bulks up from pressure. That bony prominence rubs on shoe leather and can inflame the bursa. Over time, the joint’s mechanics change. Tendons pull at the wrong angles, the sesamoids shift, the cartilage loads unevenly, and pain follows you into wider shoes and softer socks.
Biomechanics drive the progression. Some people inherit a foot shape with a mobile first ray, a relatively valgus forefoot, or a longer first metatarsal. Others pick up contributors like ligament laxity from pregnancy, repetitive load from ballet, or shoe choices that crowd the forefoot. A foot and ankle biomechanics specialist looks for these patterns. The plan to help you depends on them. If your first ray is unstable, a pad on the bump is a bandage, not a fix. If the problem sits higher up at the ankle or even the hip, addressing gait can slow the bunion’s march.
Severity is not about cosmetics. Surgeons often use angle measurements on weight-bearing X‑rays. A hallux valgus angle around the mid teens is mild, into the 20s and 30s is moderate, and beyond that is severe. Those numbers help predict whether a simple shaving procedure will fail or if a bone realignment is needed. They also correlate with symptoms, but not perfectly. I have met runners with striking angles and very little pain, and office workers with modest angles who can barely tolerate loafers. A foot and ankle pain specialist listens to both the image and the person.
What Conservative Care Can Really Do
Nonoperative care has a job: reduce pain, control inflammation, and slow progression. It does not straighten a bone that has rotated and shifted, but it can keep you functional for a long time.
Footwear is the lowest hanging fruit. Shoes with a wide toe box, a soft upper over the bump, and stable midsole give immediate relief. A shoe with a mild rocker sole unloads the forefoot at push-off and can help if the first joint aches with each step. I keep a sample pair in the clinic; the look on a patient’s face after 20 steps tells you more than any lecture.
Padding still works. Gel sleeves over the bunion reduce shear. A small spacer between the first and second toes aligns the tendons just enough to calm irritation. It is not a cure, but it quiets symptoms for many.
Custom orthotics matter when foot mechanics feed the bunion. An orthotic that supports the medial arch and stabilizes the first ray reduces the inward drift force. Off-the-shelf inserts can help, but a foot and ankle foot care specialist can tune stiffness and posting to the individual.
Therapy is not fluff. Focused exercises that strengthen the intrinsic foot muscles and improve control at the ankle and hip can change how forces cross the joint. Learning to avoid rolling inward early in stance is often worth more than any gadget. When needed, a foot and ankle tendon specialist or foot and ankle ligament specialist can address associated tendinopathies that keep the joint inflamed.
Medication has a role. Topical NSAIDs deliver anti-inflammatory effects to a hot bursa without the gastric baggage of pills. Short courses of oral NSAIDs can break a bad flare. A carefully placed corticosteroid injection into an inflamed bursa can settle pain for weeks. A foot and ankle medical doctor will help you weigh benefits and risks if diabetes, kidney disease, or other conditions are in play.
These measures work best in early or moderate bunions and when pain is the main complaint. They do less for people whose big toe is underlapping or whose second toe is dislocating at the ball of the foot. They do nothing for advanced joint arthritis. That is where a foot and ankle orthopaedic surgeon or a foot and ankle podiatric surgeon begins to make sense.
Signs You Should Talk to a Foot and Ankle Bunion Surgeon
There is no prize for enduring pain unnecessarily, and there is no reason to rush to surgery either. The timing is personal. These are the signals that push me to suggest consultation with a foot and ankle surgery expert:
- Daily pain that limits work, exercise, or basic walking despite good shoes, orthotics, and targeted therapy used consistently for at least 8 to 12 weeks. Progressive deformity, like the big toe crossing under the second, recurrent calluses beneath the second metatarsal head, or visible rotation of the toenail. Recurrent bursitis, skin breakdown, or nerve irritation over the bunion despite padding and shoe changes. Stiffness or grinding in the big toe joint that suggests cartilage injury or arthritis. Deformity that prevents fitting functional footwear for your job or sport, especially when activity defines your health or livelihood.
A foot and ankle specialist will examine your foot weight-bearing, watch your gait, and likely order standing X‑rays. If the pain pattern or exam raises suspicion for nerve involvement, a foot and ankle nerve specialist may add nerve conduction tests, though that is uncommon in straightforward bunions. Anchoring the plan to your goals matters. A nurse on 12‑hour shifts, a tennis player with tournament dates, and a retiree who gardens five mornings a week need different timelines and different trade-offs.
Who Does Bunion Surgery, and Does Training Matter?
Several professionals perform bunion surgery, and titles can confuse people. The key is scope, training, and experience with your specific problem.
Orthopaedic foot and ankle surgeons complete medical school, an orthopaedic surgery residency, then a foot and ankle fellowship. They are often labeled foot and ankle orthopaedic surgeons or foot and ankle orthopedic doctors. Podiatric surgeons complete podiatric medical school, surgical residency, and often a foot and ankle reconstructive fellowship. You will see titles like foot and ankle podiatric surgeon, foot and ankle podiatrist surgeon, or foot and ankle podiatric physician. Both tracks produce surgeons who routinely treat bunions, perform osteotomies and fusions, and manage complications. The spectrum of expertise within each field is wide.
What matters most is a surgeon’s volume and comfort with the full tool kit, from minimally invasive techniques to complex deformity correction. A foot and ankle surgeon specialist who performs several bunion procedures each week and can discuss why one technique suits your foot better than another offers more value than any title. Ask for outcomes, revision rates, and how often they perform the exact procedure they recommend for you.
In special cases, such as severe instability combined with midfoot collapse, a foot and ankle deformity specialist or foot and ankle reconstructive surgery doctor is appropriate. For diabetics with neuropathy and skin risk, a foot and ankle diabetic foot specialist or foot and ankle wound care surgeon should be in the loop.
The Menu of Surgical Options, Translated
People often come in asking for a “simple bunion shave.” That approach, called a bunionectomy or exostectomy, removes the bump but does not correct the misalignment. It is rarely sufficient on its own and tends to disappoint when the deformity recurs. Contemporary surgery aligns bones and soft tissues so the bump does not reform.
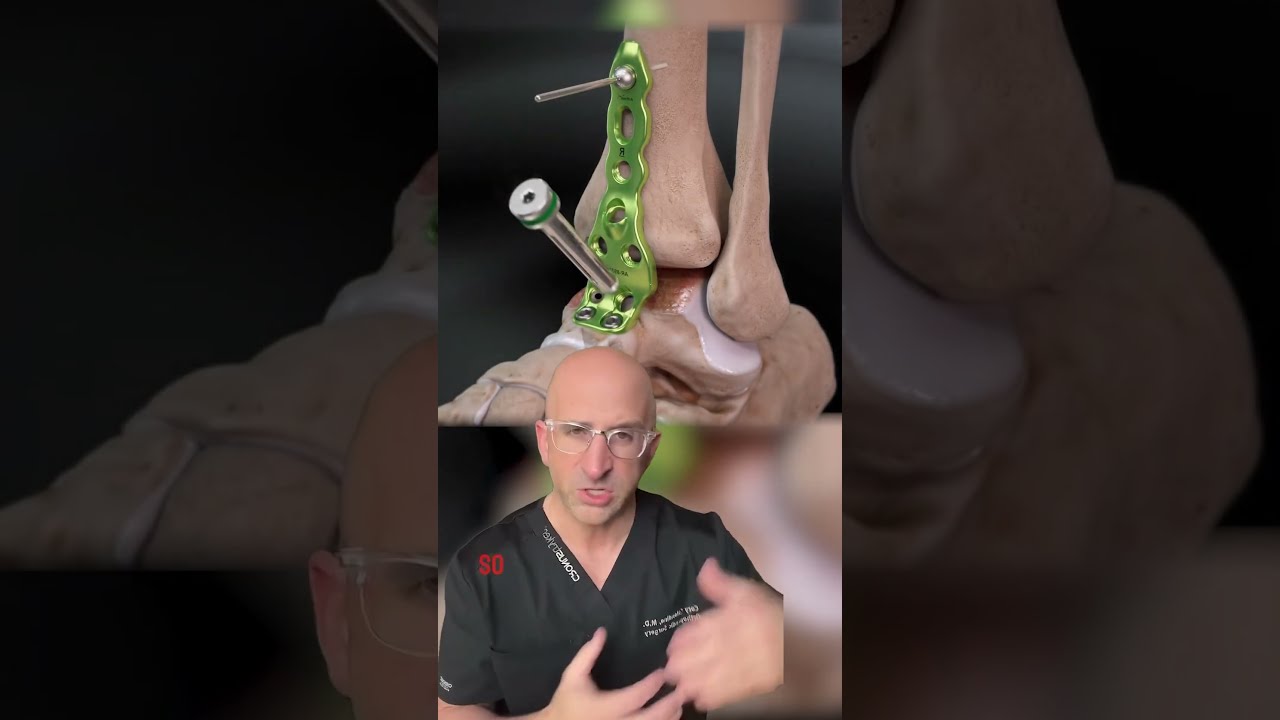
For mild to moderate bunions, distal metatarsal osteotomies do the heavy lifting. A chevron or distal osteotomy cuts the first metatarsal near the head, shifts it to align the joint, and secures it with screws. Recovery typically involves protected weight-bearing in a boot for several weeks, with a gradual return to normal shoes around 6 to 8 weeks. Many foot and ankle minimally invasive surgeons now perform this through tiny incisions using burrs and fluoroscopy. The advantage is smaller scars and potentially less soft tissue trauma. The trade-off is that it is technique sensitive. Choose a foot and ankle advanced surgeon experienced in minimally invasive methods if that approach interests you.
If the deformity is more significant or if the metatarsal has rotated, proximal osteotomies or biplanar corrections make sense. A scarf osteotomy or proximal opening wedge adds stability and allows greater correction. The rehab is similar but often a touch slower at first to protect the bone work.
When the base of the first metatarsal is unstable or the intermetatarsal angle is high, a Lapidus procedure fuses the joint at the arch where the first metatarsal meets the midfoot. This sounds extreme to patients, but stabilizing this joint straightens the toe reliably and can reduce recurrence. Expect a period of non-weight-bearing or very protected weight-bearing for a few weeks while the fusion sets. For the right foot, this procedure is a workhorse.
If the big toe joint itself is worn out, alignment alone will not solve the pain. A first metatarsophalangeal joint fusion removes the remaining cartilage and fixes the toe in a functional position for walking. People worry about losing motion. The reality, when arthritis is advanced, is that most of the motion is already gone, and fusion trades grinding pain for power at push-off. A good foot and ankle arthritis specialist or foot and ankle joint specialist will help you decide if your X‑rays and symptoms warrant this.
Soft tissue balancing accompanies most procedures. Tight lateral structures are released, the capsule is tightened medially, and the sesamoids are realigned under the first metatarsal. An experienced foot and ankle corrective surgeon does this routinely. If the second toe is unstable or hammered, a foot and ankle deformity repair surgeon may add procedures to protect the forefoot from transfer overload.
What Recovery Actually Feels Like
Timelines vary with the procedure and the person. I prefer to set ranges and milestones rather than fixed dates, because biology does not read calendars.
For distal osteotomies, most patients bear some weight in a post-op shoe or boot immediately or within a few days, keeping it light for the first two weeks to let swelling settle. Sutures come out around two weeks. By 6 to 8 weeks, many are in wide toe box sneakers. Office work is often feasible within 10 to 14 days if you can elevate the foot; standing jobs take longer. Return to light jogging begins around the two to three month mark if swelling cooperates.
For Lapidus fusions, many surgeons keep patients non-weight-bearing for two to four weeks, then progress to partial weight-bearing in a boot. It takes longer for the fusion to consolidate, so patience pays off. It is common for swelling to wax and wane for months. Push-offs feel different after a fusion, but most people adapt and regain brisk walking and hiking.
After a first MTP fusion, you cannot wear high heels beyond a modest lift. Most patients do not miss them. Hiking, cycling, rowing, and even skiing return to form. Explosive sprinting and deep squats are more nuanced and worth discussing with your foot and ankle sports medicine surgeon.
Pain control is not just pills. Elevation, ice, and compression wrapping tame swelling, which is tightly linked to pain. A foot and ankle surgical care doctor will lay out a clear regimen. Many patients use acetaminophen plus a short course of anti-inflammatories. Opioids, if used at all, should be minimal and brief. Nerve blocks during surgery can make the first day or two surprisingly comfortable.
Rehabilitation begins early. Gentle range of motion for non-fused joints, scar care, and gait training prevent bad habits. A foot and ankle mobility specialist or a seasoned physical therapist can help you progress safely.
Risks and Trade-offs, without Sugarcoating
Every operation has a risk profile, and bunion surgery is no exception. Infection rates are low, often under 2 percent in healthy nonsmokers. Nerve irritation can leave a numb patch near the incision. Most of the time it improves over months. A small number have lasting sensitivity. Bone healing is reliable in healthy patients. Smoking, uncontrolled diabetes, and certain medications slow fusion and osteotomy healing. Discuss these with your foot and ankle medical expert before scheduling.
Caldwell NJ foot and ankle surgeon Essex Union Podiatry, Foot and Ankle Surgeons of NJRecurrence is the risk most people fear, and rightfully so. It is not just bad luck. Under-correction, unstable first ray mechanics, and ignoring rotation lead to a persistent deformity. Choosing the right operation for your foot and following post-op guidance reduce that risk substantially. I have revised operations done elsewhere that failed because the wrong lever was pulled. That is another reason to favor a foot and ankle surgeon expert who can explain their reasoning and show before-and-after outcomes.
Stiffness can follow any surgery, especially if swelling persists for weeks. Working on motion and scar pliability early helps. Hardware occasionally bothers people. Screws or plates can be removed once bones are solid if they irritate.
Cosmetics improve, but I caution patients not to chase a narrow, straight aesthetic at the expense of function. A healthy big toe points modestly inward and carries load. The best operations respect that.
Choosing the Right Foot and Ankle Specialist for You
Credentials open the door. Chemistry and communication close the deal. You want a foot and ankle consultant who listens, examines you with curiosity, and is comfortable saying both “you are not ready for surgery” and “surgery is your best tool now.”
Bring the shoes and inserts you actually wear. A foot and ankle foot specialist can learn a lot from outsole wear patterns. Ask how many of your surgeon’s cases are bunions, what procedures they perform most, and what they recommend for your specific angles and symptoms. A foot and ankle musculoskeletal surgeon who treats the whole chain from hip to toes will catch gait issues that feed recurrence.
If you are an athlete, a foot and ankle sports surgeon can tailor the plan to your season and sport. Ballet dancers, field sport athletes, and hikers place different demands on the first ray. If you have systemic arthritis, a foot and ankle cartilage specialist or foot and ankle arthritis specialist will integrate systemic management. For neuropathy or vascular issues, loop in a foot and ankle trauma doctor or foot and ankle wound care surgeon early if skin integrity is a concern.
Second opinions are fair, especially when recommendations differ. It is common for one foot and ankle corrective surgery specialist to favor minimally invasive chevrons while another suggests a Lapidus for the same X‑ray. The right answer lives in the details of your exam and goals.
Realistic Expectations: Results by the Numbers
Satisfaction rates after modern bunion surgery are high, often quoted in the 80 to 90 percent range. People report less pain, better shoe options, and improved function. Return to most daily activities happens by two to three months, with swelling and shoe choices continuing to improve for up to a year. Runners frequently return to prior mileage; pivoting sports depend on stability and patience.
Minimally invasive techniques show promising outcomes comparable to open methods in properly selected patients, with smaller incisions and potentially faster early comfort. The final alignment and recurrence rates track the surgeon’s skill and the matching of procedure to deformity more than the size of the incision.
Work with your foot and ankle surgical specialist to define success in your terms. “I want to walk five miles without limping.” “I need to stand all day in the OR.” “I want to fit my hiking boots again.” Those are measurable and meaningful.
Special Situations Worth Calling Out
Pediatric and adolescent bunions behave differently. A foot and ankle pediatric surgeon will be cautious about operating before growth plates close unless pain or rapid progression forces the issue. Shoe wear and activity modification are first-line.
Hypermobile patients and those with connective tissue disorders face higher recurrence. A foot and ankle instability surgeon will consider more proximal stabilization like a Lapidus earlier.
Diabetic patients with neuropathy need extra care. A foot and ankle diabetic foot specialist will coordinate blood sugar control and pay attention to wound risk. Offloading, skin care, and footwear are critical before and after surgery.
If your bunion coexists with flatfoot or calf tightness, address them together. A tight calf drives forefoot overload. Stretching, night splints, or even a small calf lengthening combined with bunion correction can prevent transfer pain. A foot and ankle Achilles tendon surgeon or foot and ankle plantar fasciitis specialist may be part of the plan if heel and arch pain complicate the picture.
Cost, Time, and Practical Planning
Most insurers cover bunion surgery when pain and functional limits are documented and conservative measures have failed. Prior authorization is common. Gather notes from your foot and ankle treatment doctor detailing attempts at nonoperative care. Expect facility, surgeon, and anesthesia fees. High-deductible plans merit a candid conversation with the billing team.
Time off work varies. Desk jobs might require one to two weeks of modified duty with foot elevation, then a gradual return. Jobs that require prolonged standing or ladder climbing need more time, often six to eight weeks before long shifts feel possible. Build a plan for rides, meal prep, and tasks that require two hands, especially if you will be non-weight-bearing initially. A knee scooter or iWalk crutch can be a game changer.
A Short Checklist for Your Surgical Consultation
- Bring your three most-worn pairs of shoes and any inserts or orthotics. Write down your top three functional goals and your timeline constraints. Ask the surgeon to explain why a specific procedure matches your foot and what the alternatives are. Clarify weight-bearing rules, driving restrictions, and expected time to your key activities. Discuss how swelling and pain will be managed during the first four weeks, and who to call after hours.
When Surgery is Not the Right Move
Sometimes the bunion is not the main pain generator. Nerve entrapment, stress fractures, or inflammatory arthritis may masquerade as bunion pain. A careful foot and ankle medical specialist will rule those out. Other times the bunion is real, but life timing is bad. Major travel, a new job, caregiving responsibilities, or poor diabetes control argue for holding off. In those cases, maximize conservative care and revisit surgery when circumstances shift.
There are also feet where alignment on X‑ray looks dramatic, but the person is comfortable and functional. If your pain is minimal and your activities are intact, there is no law that says you must fix a bunion because it looks crooked. A foot and ankle consultant worth your trust will say so.
The Bottom Line
A foot and ankle bunion surgeon becomes the right choice when pain persists despite smart nonoperative care, when deformity progresses, or when the joint itself has become arthritic. The operation should match your foot’s anatomy and your life’s demands, not a trend on social media. Whether you land with a foot and ankle orthopaedic surgeon or a foot and ankle podiatric surgery expert, focus on experience, outcomes, and a shared plan you understand.
Start with the basics: shoes that fit the foot, not the other way around. Add targeted therapy and orthotics when mechanics call for them. If those steps no longer keep pace with your pain or if your big toe is wandering, sit down with a foot and ankle specialist doctor who can walk you through options. Relief is not theoretical. I have watched hikers reclaim trails, chefs finish dinner service without glancing at the clock, and grandparents crouch for photos instead of searching for a chair. With the right partner and a clear plan, your bunion does not have to set your limits.